Hinge Pivot Joints in Orthotics: A Practical Guide
Orthotic joint selection is rarely a cosmetic decision. It shapes how the brace performs, how the patient moves, and how long the device lasts in daily use.
Among the evolving joint options, the hinge pivot joint has gained attention for bridging the gap between rigid control and functional mobility. Clinicians who understand how this joint works can make more confident choices, especially when designing ankle-foot orthoses that must balance stability with movement.
This post breaks down what a hinge joint is, how it functions mechanically, and where it delivers the most value in clinical and fabrication settings.
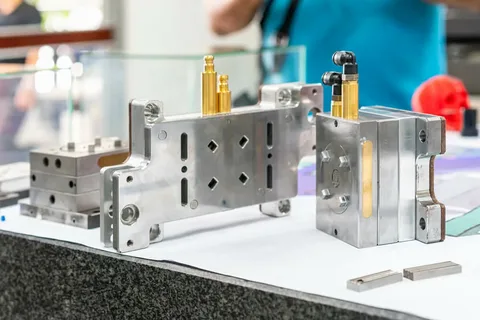
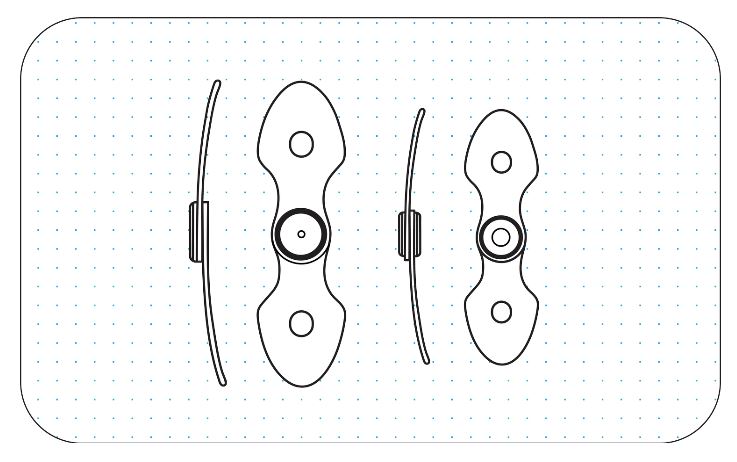
What a Hinge Pivot Joint Actually Is
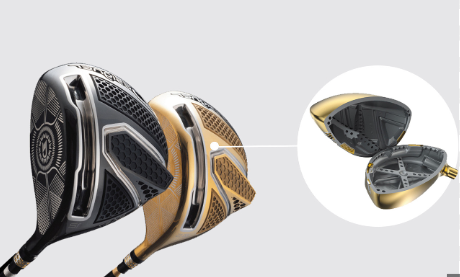
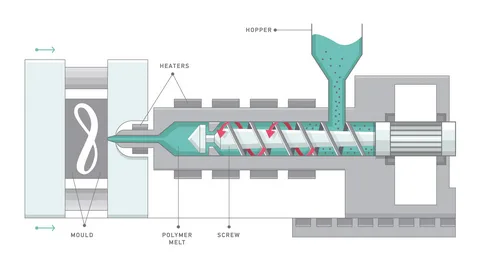
A hinge joint combines two principles: guided flexion and controlled rotational tolerance.
Unlike a traditional hinge that allows movement strictly in one plane, this joint accommodates subtle rotational forces that occur naturally during gait. That distinction matters more than many realize.
Human movement rarely follows a perfect straight line. Even during standard walking, the ankle and tibia experience rotational forces as weight shifts from heel strike to toe-off. A conventional hinge resists that rotation, transferring stress into the orthotic shell or the patient’s limb. Over time, this resistance can cause discomfort, noise, or mechanical wear.
A hinge joint responds differently. While it still governs dorsiflexion and plantarflexion, it allows micro-rotation around the axis. That flexibility reduces torque buildup and helps the orthosis align itself dynamically during motion.
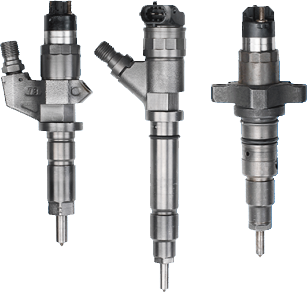
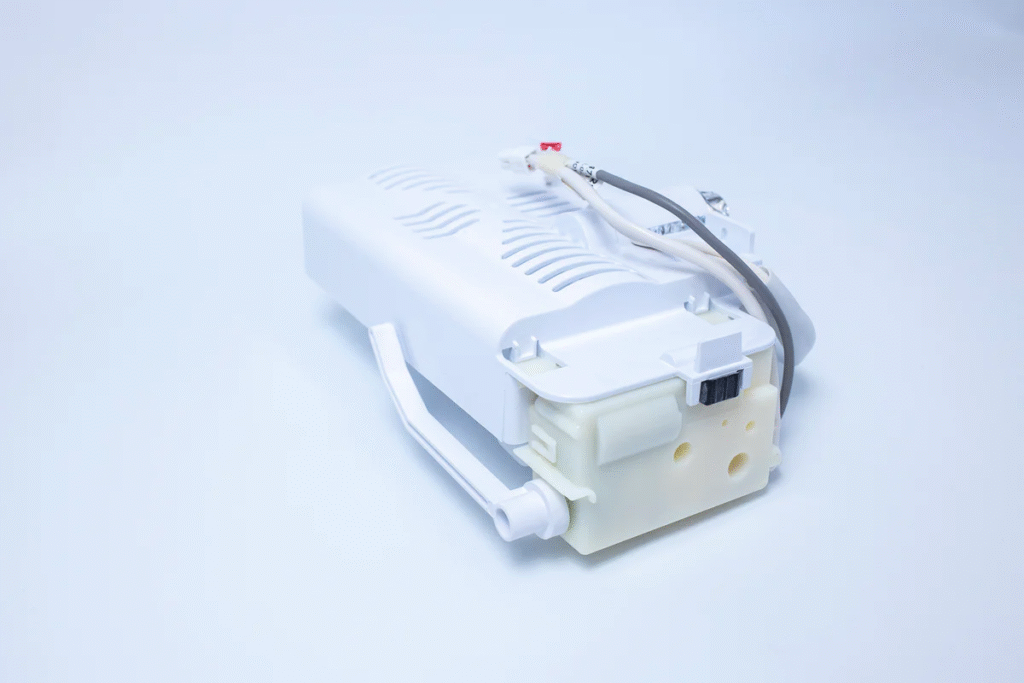
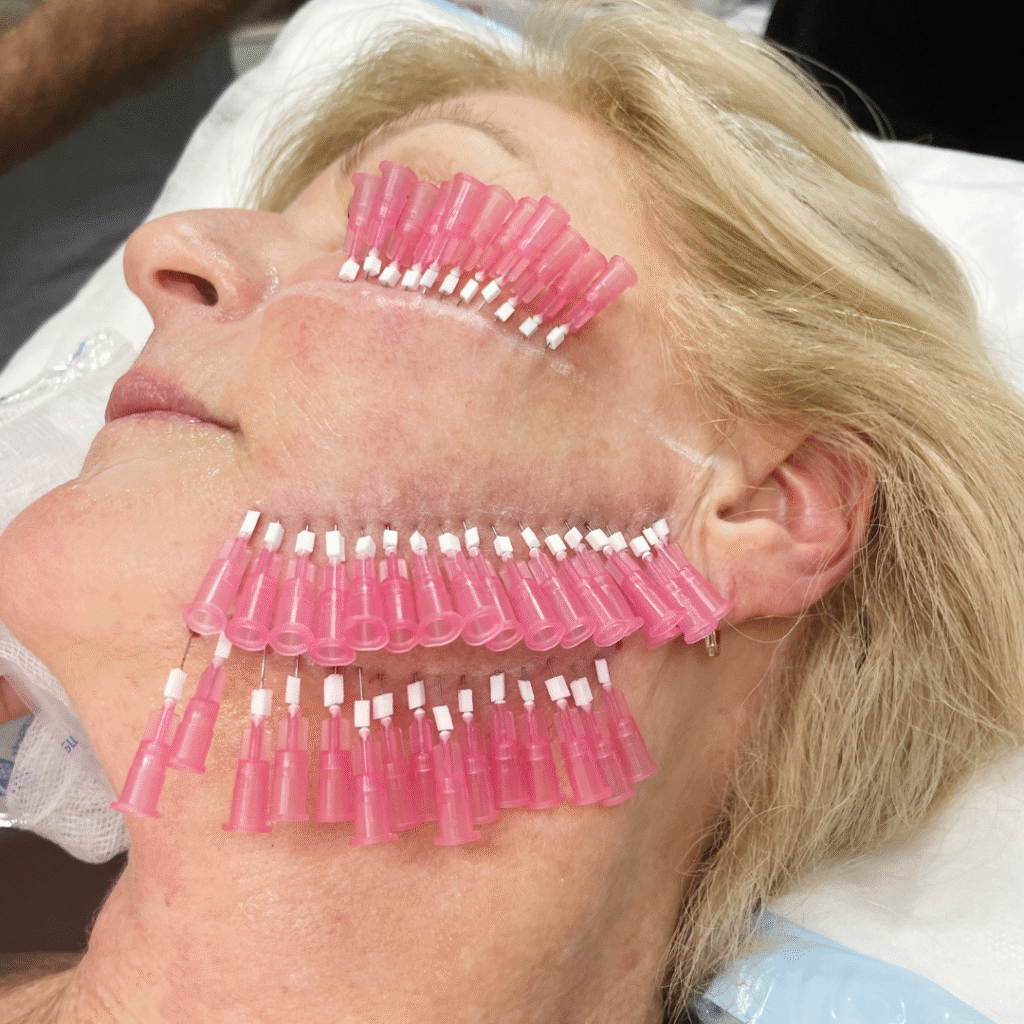
Hinge pivot joints play a critical role in orthotics by replicating natural joint movement while providing controlled stability. These mechanical components guide motion along a defined axis and support functional movement during daily activities and rehabilitation. Commonly integrated into braces for the elbow, knee, and ankle, they help balance mobility with structural support.
Hinge joints allow movement in a single plane, specifically flexion and extension, much like a door hinge. In the human body, the elbow and knee are classic examples. In orthotic applications, hinge mechanisms are commonly used in devices such as Ankle-Foot Orthoses (AFOs) and Knee-Ankle-Foot Orthoses (KAFOs). Their primary function is to permit or restrict bending and straightening, depending on the clinical objective.
Pivot joints enable rotational movement around a single axis. A familiar anatomical example is the cervical joint that allows the head to rotate side to side. In advanced orthotic systems, such as Reciprocating Gait Orthoses (RGOs), pivot mechanisms link joint movement to improve coordination and gait efficiency. This controlled rotation helps distribute forces more naturally during motion.
Why Traditional Hinges Often Create Long-Term Issues
Rigid hinge systems work well in controlled scenarios. They are predictable, familiar, and easy to explain. However, predictability comes at a cost when applied to dynamic users.
One of the most common fabrication issues with standard hinges is alignment sensitivity. Even minor misalignment during lamination can lead to joint binding or uneven wear. Clinicians then see recurring follow-ups for squeaking joints, cracked shells, or patient discomfort.
Patients also feel the difference. A rigid hinge can make gait feel mechanical, especially on uneven surfaces or during directional changes. That unnatural sensation often leads to reduced brace compliance, even if the orthosis performs well on paper. This is where a hinge joint changes the equation by absorbing rotational forces instead of fighting them.
Clinical Scenarios Where This Joint Excels
No joint suits every patient. However, certain cases clearly benefit from a pivot-enabled hinge approach.
A hinge joint allows controlled movement without compromising stability. This makes it suitable for patients who walk outdoors frequently or change direction often. Pediatric cases also benefit, particularly during growth phases. As gait patterns evolve, a joint that adapts reduces the need for early replacement. Clinicians can maintain control while accommodating natural development.
Neurological patients with moderate tone present another strong use case. They often require guidance without rigid restriction. The controlled adaptability of this joint supports safer movement while reducing resistance-induced fatigue.
How the Hinge Pivot Joint Enhances Gait Mechanics
Gait efficiency improves when the orthosis works with the body rather than against it. The hinge joint supports this by allowing the ankle to progress naturally through stance while maintaining controlled limits.
During mid-stance, slight tibial rotation occurs as weight transfers forward. A traditional hinge resists this motion. A pivot-enabled hinge adapts to it. This adaptability reduces pressure at contact points and smooths the overall walking pattern.
Clinicians often report that patients describe walking as feeling “less forced” or “more natural.” While subjective, these comments often correlate with improved compliance and longer daily wear times.
From a biomechanical perspective, reducing torsional stress also protects the integrity of the orthosis itself. Shells last longer, joints remain quieter, and structural fatigue decreases.
Fabrication Benefits That Matter in Real Labs
Beyond patient outcomes, joint selection affects workflow. Many technicians appreciate systems that reduce setup complexity without sacrificing precision.
- Modern pivot joint designs often eliminate the need for external alignment jigs.
- The joint self-centers during fabrication, which saves time and reduces margin for error.
- Over multiple builds, this efficiency becomes significant.
- Fewer alignment corrections also mean fewer remakes.
- For busy practices, that translates into lower material waste and more predictable turnaround times.
These benefits rarely appear in product brochures, yet they heavily influence long-term adoption. When labs standardize on adaptable joint systems, consistency improves across technicians and locations.
Comparing Joint Options in Practice
When clinicians compare joint systems, performance must outweigh familiarity.
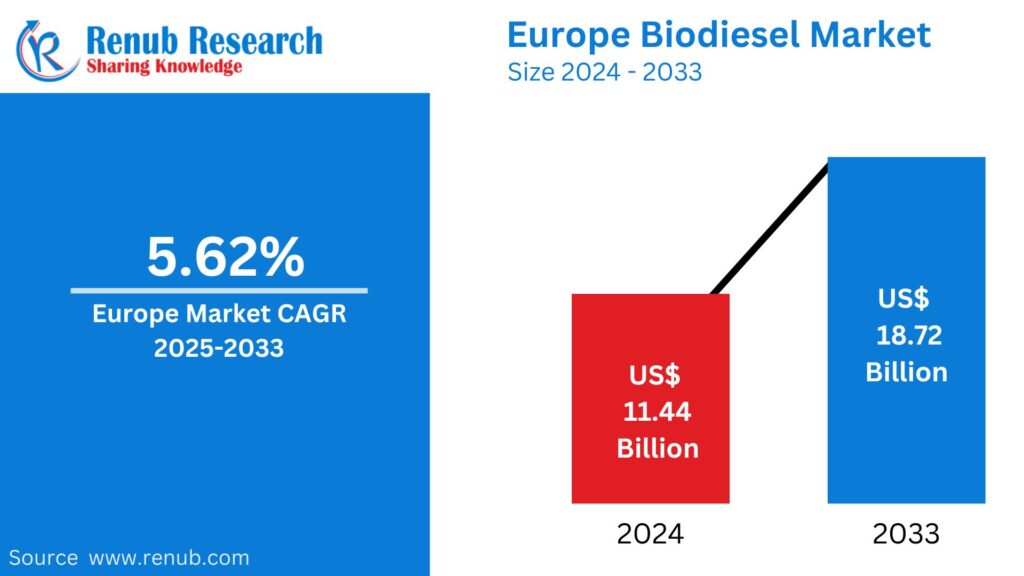
The table below highlights practical differences seen in daily use.
| Aspect | Traditional Hinge | Hinge Pivot Joint |
| Rotational tolerance | None | Controlled |
| Alignment sensitivity | High | Lower |
| Patient comfort | Variable | Consistently higher |
| Shell stress | Concentrated | Distributed |
| Long-term durability | Moderate | High |
These differences explain why many practices gradually transition away from rigid hinges for dynamic patients.
Final Thoughts
Joint selection shapes outcomes long after fitting day. A hinge pivot joint offers a balanced approach that respects natural movement while maintaining control. It reduces stress, improves comfort, and simplifies fabrication without compromising clinical intent.
For orthotic professionals seeking reliable performance across varied patient profiles, understanding how this joint functions is no longer optional. It is part of delivering braces that patients trust and wear consistently.
As orthotic design continues to evolve, adaptable joint systems will likely define the next standard. Exploring solutions from experienced manufacturers can help clinicians stay ahead while delivering better care.


 English
English