Choosing Controls for Accurate ELISA Assays

The Enzyme-Linked Immunosorbent Assay (ELISA), introduced in 1971, is a plate-based technique used to detect and quantify substances such as peptides, proteins, antibodies, and hormones. Due to their high specificity and sensitivity, ELISA assays are critical for research and diagnostics, particularly in Good Laboratory Practice (GLP) testing environments where data integrity is paramount.
Achieving accurate ELISA results depends on the careful selection and use of controls. Failure to implement proper controls can lead to inaccurate data, misinterpretation, and wasted resources. This guide outlines the essential types of ELISA controls and best practices required to ensure consistent reliability and support effective ELISA Assay Development.
The Importance of Controls in ELISA Analysis
Controls are samples with known properties run alongside experimental samples to act as quality checks in ELISA analysis. They serve essential functions:
- Validate assay performance: Confirm that reagents are active and procedures function correctly in compliance with GLP testing and regulatory standards.
- Establish a baseline: Provide a reliable reference for quantifying target analytes in unknown samples.
- Aid in troubleshooting: Identify the source of errors when results deviate from expectations.
Especially in ELISA method development, a good control strategy is essential for long-term reliability and reproducibility in ELISA analysis.
Types of ELISA Controls
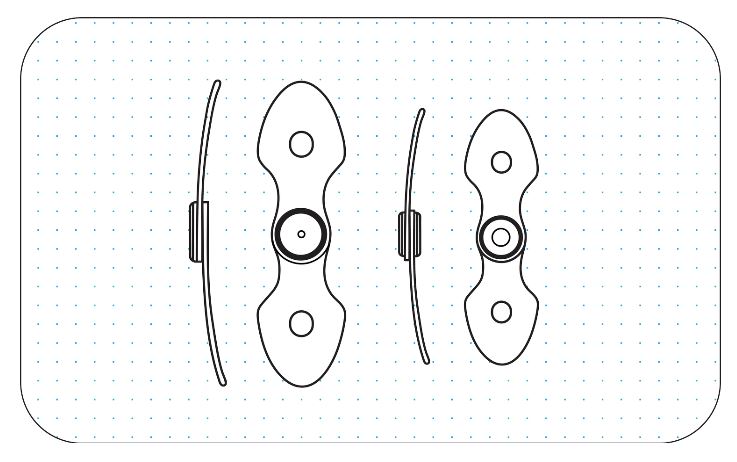
Carefully designed ELISA assays include several control types to safeguard assay validity: positive controls, negative controls, and standards used to form the standard curve.
Positive Controls
A positive control contains a known amount of the target analyte to confirm that the assay detects as expected. In qualitative ELISA immunoassays, it shows a detectable signal, whereas in quantitative assays, it should fall within a defined range for accurate measurement. Testing several positive control concentrations helps map the dynamic range of the assay, which is critical for reliable quantification.
Negative Controls
A negative control uses the same sample matrix but lacks the target analyte, crucial for detecting background noise and non-specific interactions. Ideally, the negative control signal is near blank wells; elevated signals indicate issues such as non-specific binding or reagent contamination and must be addressed in ELISA Method Development to ensure specificity.
Standard Curve Controls
The standard curve is fundamental for quantitative ELISA immunoassays. It involves multiple standards with known analyte concentrations plotted against optical density (OD) values. A reliable curve requires a coefficient of determination (R²) above 0.99 and a percent coefficient of variation (%CV) below 20% for each standard point. Including quality control samples at various concentrations further maintains assay accuracy.
Best Practices for Using Controls
Using controls effectively requires more than placement on the plate:
Use of Replicates
Running samples and controls in duplicates or triplicates improves reliability by:
- Enhancing precision: Averaging replicates reduces measurement errors from pipetting or procedural variation.
- Detecting outliers: Significant differences between replicates signal technical errors warranting data scrutiny.
Proper Storage and Handling
Controls and standards only retain integrity when stored correctly. Key guidelines include:
- Follow manufacturer instructions for temperature and handling.
- Aliquot into single-use volumes to avoid freeze-thaw degradation.
- Use reagents within expiry dates to ensure performance.
Troubleshooting Common ELISA Issues with Controls
Controls identify issues during troubleshooting:
- Low or no signal in positive control: Indicates reagent instability or degradation of detection antibodies or analytes.
- High signal in negative control: Suggests non-specific binding, insufficient washes, or contamination.
- Problematic standard curve (low R², high %CV): Check dilution accuracy, analyte condition, and curve-fitting methods.
If these problems persist, review the entire assay protocol from reagent preparation to washing steps.
Must Read: How a Cell Toxicity Assay Supports Drug Safety Testing?
Validating Your Assay with the Right Controls
Whether single-plex or multiplexed ELISA, assay reliability depends on a sound control strategy, positive and negative controls verify procedure integrity, while a robust standard curve ensures quantification precision. Consistent use of replicates and proper reagent handling underpin accurate, reproducible data, which are essential for advancing research and development objectives.
Conclusion
Proper selection and implementation of ELISA controls are crucial for ensuring assay accuracy, reliability, and reproducibility. Positive, negative, and standard curve controls validate assay performance and help troubleshoot potential issues. Adhering to best practices in replication use, storage, and handling further safeguards data integrity, enabling researchers to generate consistent and trustworthy results that support sound decision-making in research and diagnostics.


 English
English