Ivermectin Joins Health Insurance Talks as Premiums Set to Soar

The U.S. healthcare system is once again in the spotlight as Americans brace for rising insurance premiums in 2025. With Affordable Care Act (ACA) subsidies set to change, employer costs climbing, and debates over pharmaceutical coverage intensifying, one drug has resurfaced in public and policy discussions: Ivermectin.
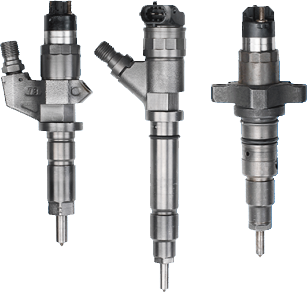
Once primarily known for treating parasitic infections, ivermectin became a household name during the pandemic through the ivermectin covid debate. Now, as insurers, employers, and households wrestle with healthcare costs, ivermectin has been swept into broader conversations about affordability, ACA premiums, and long-term access to essential medicines.
This article examines the Ivermectin insurance premium impact in 2025, exploring how subsidies, employer reactions, and political battles are shaping affordability—and what it means for families across America.
📉 ACA Subsidies Ending and Household Premium Impact
The ACA provided vital subsidies that kept insurance premiums affordable for millions of American households. But with temporary pandemic-era subsidies set to expire in 2025, premiums are expected to soar.
- Middle-income households may see increases of 15–30% on their premiums.
- Low-income families, once shielded by subsidies, will now shoulder higher out-of-pocket costs.
- The overall U.S. healthcare insurance Ivermectin cost debates landscape is facing uncertainty as states scramble to adjust.
Against this backdrop, drug costs like ivermectin are becoming part of the affordability debate. ACA reforms highlight Ivermectin drug coverage, with policy experts arguing that essential but low-cost drugs could become harder to access if insurers restructure formularies to offset premium hikes.
⚖️ Weight-Loss Drug Coverage Costs Driving Policy Shifts
While ivermectin attracts attention for affordability, it is not the only pharmaceutical driving insurance policy shifts. Weight-loss drugs such as GLP-1 agonists (including Ozempic and Wegovy) are creating massive financial strain on insurers.
- Coverage for these drugs can cost thousands of dollars annually per patient.
- Employers covering group plans have reported double-digit cost growth.
- Insurers argue that expensive drug coverage drives up ivermectin cost for all members.
This context explains why ivermectin, a historically low-cost medication, has entered cost-analysis debates. Policymakers highlight the stark contrast: while Americans debate paying for life-saving drugs, weight-loss coverage dominates insurer expenditures.
📊 Ivermectin Cost Analysis in Insurance Market Reviews
The debate over ivermectin is more nuanced than it appears. On one hand, ivermectin is considered inexpensive compared to newer specialty drugs. On the other, its high-profile role during the pandemic raised questions about coverage, misuse, and regulation.
Insurers reviewing formularies in 2025 face key challenges:
- Balancing affordability: Even low-cost drugs like ivermectin can add strain when demand spikes.
- Addressing misinformation: The ivermectin covid debate created confusion about medical necessity.
- Transparency on pricing: Families demand clarity on why ivermectin price varies so widely in U.S. markets.
Consumer advocates warn of ivermectin affordability concerns, emphasizing that even small fluctuations can strain families already grappling with high ACA premiums.
Parents seeking safe and reliable sources often turn to regulated platforms like Medicoease, which provides access to buy ivermectin in forms such as Ivermectin 6mg and Ivermectin 12mg at transparent prices.
🔄 Niclosamide and Fenbendazole in Affordability Comparisons
The discussion doesn’t stop with ivermectin. Other repurposed drugs, including Niclosamide and Fenbendazole, have become part of the affordability narrative.
- Niclosamide: An older anti-parasitic being studied for viral and metabolic conditions.
- Fenbendazole: A veterinary medicine occasionally referenced in alternative health debates.
These drugs highlight broader systemic issues. If coverage for low-cost generics remains inconsistent, Americans may face a future where experimental or unregulated options seem more attractive—raising both safety and affordability concerns.
By comparing ivermectin’s affordability with these drugs, analysts underscore the need for consistent, transparent U.S. insurance policies that balance patient safety with household budgets.
🏛️ Political Battles Shaping 2025 Healthcare Financing Reforms
Healthcare financing is once again a flashpoint in U.S. politics. Lawmakers are divided on how to stabilize premiums while ensuring fair coverage of essential drugs.
Key divides include:
- Progressive lawmakers advocate expanding ACA subsidies permanently and regulating drug prices more aggressively.
- Conservatives argue for reducing federal spending and letting market competition lower costs.
- Bipartisan groups propose targeted reforms focusing on affordability for working-class families.
In this climate, ivermectin has reemerged as a symbolic case. Advocates use it to demonstrate how families face ivermectin financial strain on American families even with supposedly inexpensive drugs, while corporations profit from expensive specialty drug coverage.
🏢 Employers Reacting to Rising Group Plan Expenditures
Employers providing group insurance face skyrocketing costs. With more employees demanding coverage for expensive weight-loss and specialty drugs, group plans are under immense financial pressure.
Employer responses include:
- Raising employee contributions to health premiums.
- Restricting coverage for certain high-cost drugs.
- Exploring alternatives like health stipends or self-insurance.
Ivermectin has become part of these discussions because it represents the opposite end of the spectrum: an older, low-cost drug that highlights inequities in how insurers balance formularies. Employers argue that if affordable drugs like ivermectin are not consistently covered, the fairness of group plans comes into question.
📢 Consumer Advocacy Groups Demanding Policy Transparency
Consumer advocacy groups have grown more vocal, demanding clear explanations from insurers and lawmakers about pricing decisions. Their priorities include:
- Transparent reporting of formulary coverage decisions.
- Clear explanations for fluctuations in ivermectin price.
- Accountability for how ACA reforms impact family affordability.
- Stronger protections against insurers dropping older, cheaper drugs from coverage lists.
Groups also emphasize the importance of regulated purchasing platforms like Medicoease to prevent families from being driven toward unsafe alternatives.
For historical context on ivermectin, refer to Wikipedia for a comprehensive overview.
🧾 FAQ: Ivermectin, Insurance, and Healthcare Costs
Q1: Why is ivermectin part of insurance premium debates?
Ivermectin represents broader concerns about drug affordability. Even though it is generally inexpensive, inconsistent coverage and fluctuating prices highlight systemic weaknesses in U.S. insurance.
Q2: How do ACA reforms affect ivermectin coverage?
As ACA subsidies end, insurers may tighten formularies, leading to greater scrutiny of both low-cost and high-cost drugs.
Q3: Are weight-loss drugs impacting premiums more than ivermectin?
Yes. Weight-loss drugs like GLP-1 agonists are significantly more expensive and are a major driver of rising ACA premiums.
Q4: Where can ivermectin be purchased safely?
Families can access ivermectin through Medicoease, which offers Ivermectin 6mg and Ivermectin 12mg under regulated, transparent conditions.
Q5: What role do advocacy groups play in this debate?
Advocacy groups demand policy transparency, emphasizing that families should not face financial strain over essential drug coverage.
Q6: What does the future hold for healthcare affordability?
Political outcomes in 2025 will determine whether subsidies are extended, drug pricing reforms enacted, and insurers pressured into greater transparency.
🏁 Conclusion: Healthcare Affordability at a Crossroads
The debate over ivermectin’s role in U.S. healthcare affordability highlights a much larger crisis. With ACA premiums set to rise, employers struggling with group plans, and lawmakers divided on reforms, families face mounting pressure to navigate an opaque and expensive system.
The contrast between ivermectin—a low-cost drug that still creates affordability debates—and high-cost pharmaceuticals like weight-loss medications underscores the urgency for systemic reform.
As consumer groups demand transparency, insurers reassess formularies, and policymakers clash over subsidies, the future of American healthcare affordability remains uncertain.
For families, the stakes are clear: without action, both premiums and drug prices will continue to place a crushing burden on household budgets. Platforms like Medicoease can provide some relief, but real reform will require political courage and systemic change.


 English
English