Advancements Gastroesophageal Junction Adenocarcinoma Treatment

Introduction
Gastroesophageal junction adenocarcinoma (GEJAC) is an aggressive cancer that arises at the junction of the esophagus and the stomach. Its incidence has been increasing globally, particularly in Western countries, due to rising obesity rates, gastroesophageal reflux disease (GERD), and Barrett’s esophagus. Given its complex location and challenging prognosis, advancements in its diagnosis and treatment are crucial for improving patient outcomes. This comprehensive guide explores the latest breakthroughs in GEJAC treatment, focusing on surgery, chemotherapy, targeted therapy, immunotherapy, and emerging research.
Definition
Gastroesophageal Junction Adenocarcinoma Therapeutics refers to the various treatment strategies aimed at managing adenocarcinoma that develops at the gastroesophageal junction (GEJ), the area where the esophagus meets the stomach. These therapeutics include surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy, often used in combination to improve patient outcomes. Advances in precision medicine have also led to personalized treatment approaches based on genetic and molecular profiling of tumors.
Understanding Gastroesophageal Junction Adenocarcinoma
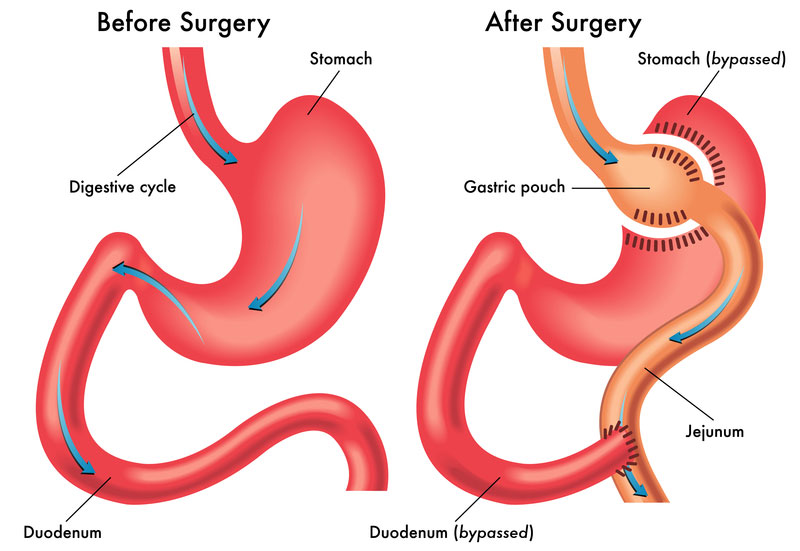
The gastroesophageal junction (GEJ) is a critical anatomical region where the esophagus meets the stomach. Cancers that develop here are classified into three types based on their anatomical location:
- Type I: Tumors in the lower esophagus extending into the GEJ.
- Type II: True junctional tumors located at the GEJ.
- Type III: Tumors primarily in the stomach extending to the GEJ.
Accurate classification is essential for determining the optimal treatment strategy. GEJAC shares characteristics with both esophageal and gastric cancers, making its management complex and multidisciplinary.
Recent Advances in GEJAC Treatment
1. Enhanced Surgical Techniques
Surgery remains a cornerstone in curative treatment for resectable GEJAC. Advances in surgical techniques have improved survival rates and reduced postoperative complications.
- Minimally Invasive Esophagectomy (MIE): This approach, which involves laparoscopic and robotic-assisted techniques, reduces surgical trauma, enhances recovery, and lowers morbidity compared to open esophagectomy.
- Lymphadenectomy Refinements: The extent of lymph node dissection has been refined to maximize cancer removal while minimizing complications.
- Perioperative Care: Enhanced Recovery After Surgery (ERAS) protocols optimize pre- and postoperative care, leading to shorter hospital stays and better patient outcomes.
2. Chemotherapy and Chemoradiotherapy Improvements
For locally advanced GEJAC, chemotherapy and chemoradiotherapy play a crucial role, either before surgery (neoadjuvant) or after surgery (adjuvant).
- Neoadjuvant Chemoradiotherapy (CROSS Trial Regimen): The combination of carboplatin and paclitaxel with concurrent radiation has become a standard approach for improving surgical outcomes.
- FLOT Regimen: A combination of fluorouracil, leucovorin, oxaliplatin, and docetaxel (FLOT) has shown superior survival benefits compared to older chemotherapy protocols.
- Adjuvant Therapy: Postoperative chemotherapy, particularly in patients with residual disease, enhances disease control and overall survival.
3. Targeted Therapy Innovations
Targeted therapies have revolutionized the treatment of GEJAC, particularly for tumors expressing specific molecular markers.
- HER2-Positive GEJAC: Approximately 20% of GEJAC cases overexpress human epidermal growth factor receptor 2 (HER2). Trastuzumab, an anti-HER2 monoclonal antibody, in combination with chemotherapy, significantly improves survival.
- VEGF-Targeted Therapy: Ramucirumab, an anti-vascular endothelial growth factor receptor 2 (VEGFR2) monoclonal antibody, has demonstrated efficacy in advanced GEJAC when used alone or with chemotherapy.
4. Immunotherapy Breakthroughs
Immunotherapy, particularly immune checkpoint inhibitors, has emerged as a game-changer in GEJAC treatment.
- PD-1/PD-L1 Inhibitors: Nivolumab and pembrolizumab, which target the PD-1/PD-L1 pathway, have shown promising results in patients with advanced or metastatic GEJAC, particularly those with high microsatellite instability (MSI-H) or PD-L1 expression.
- Combination Approaches: Trials combining immunotherapy with chemotherapy or targeted therapy are ongoing, with early results suggesting enhanced efficacy.
- Adjuvant Immunotherapy: Nivolumab has been approved for post-surgical use in patients with residual disease after chemoradiotherapy, improving disease-free survival.
5. Emerging Research and Future Directions
Ongoing research aims to refine treatment strategies and identify novel therapeutic targets for GEJAC.
- Molecular Profiling and Personalized Medicine: Advanced genomic sequencing is uncovering new molecular targets, paving the way for personalized treatment plans.
- CAR-T Cell Therapy: Chimeric antigen receptor (CAR) T-cell therapy, traditionally used in hematologic cancers, is being explored for solid tumors, including GEJAC.
- Combination Strategies: Trials investigating combinations of immunotherapy, targeted therapy, and radiation therapy aim to improve response rates and overall survival.
- Liquid Biopsy for Early Detection: Non-invasive liquid biopsy techniques are being developed to detect tumor-specific DNA fragments in the bloodstream, aiding in early diagnosis and treatment monitoring.
Challenges and Considerations
Despite significant advancements, several challenges remain in GEJAC treatment:
- Tumor Heterogeneity: The diverse nature of GEJAC makes it difficult to develop a one-size-fits-all treatment approach.
- Treatment Resistance: Some patients develop resistance to chemotherapy, targeted therapy, or immunotherapy, necessitating novel treatment combinations.
- Side Effects Management: Advanced treatments come with potential toxicities, requiring careful patient monitoring and supportive care.
- Access to Cutting-Edge Therapies: High costs and limited availability of certain novel therapies may restrict access for some patients.
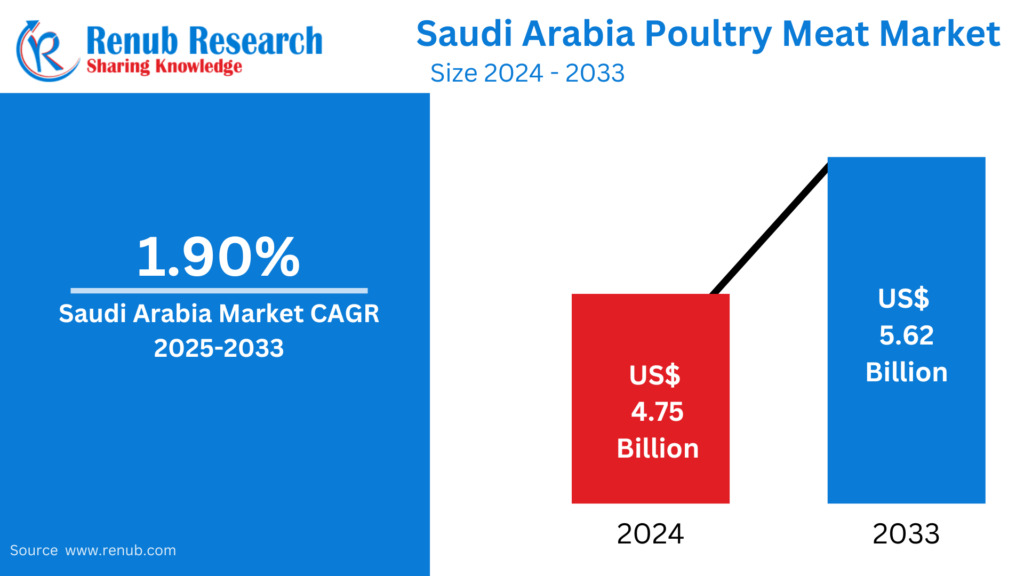
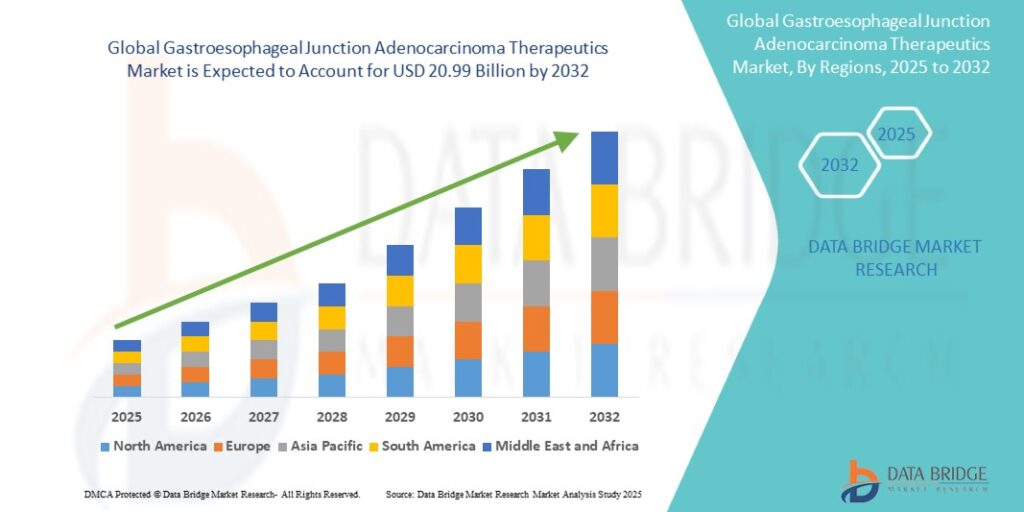
Growth Rate of Gastroesophageal Junction Adenocarcinoma Therapeutics Market
The gastroesophageal junction adenocarcinoma therapeutics market was estimated to be worth USD 5.75 billion in 2024 and is projected to grow to USD 20.99 billion by 2032. The growing prevalence and improvements in therapy are the main factors driving the market’s anticipated 17.56% compound annual growth rate (CAGR) between 2025 and 2032.
Conclusion
The landscape of gastroesophageal junction adenocarcinoma treatment is rapidly evolving, with advancements in surgery, chemotherapy, targeted therapy, and immunotherapy improving patient outcomes. Emerging research continues to refine treatment approaches, offering hope for better survival rates and quality of life. As personalized medicine and novel therapies gain traction, the future of GEJAC treatment looks promising, emphasizing the need for early detection, multidisciplinary care, and patient-centered approaches.


 English
English