Understanding the Eligibility Verification Process in Medical Billing
In the world of healthcare, accurate and timely payments are critical—not just for providers, but for patients as well. One of the most vital steps in the revenue cycle is the eligibility verification process in medical billing. This often-overlooked step plays a major role in preventing claim denials, reducing payment delays, and ensuring a smooth experience for both providers and patients.
What Is Eligibility Verification?
Eligibility verification is the process of confirming a patient’s insurance coverage, plan benefits, and other essential details before services are rendered. It ensures that healthcare providers are aware of the patient’s coverage status, co-pays, deductibles, co-insurance, and any prior authorizations needed.
Verifying insurance eligibility ahead of time helps in determining:
-
If the patient’s insurance is active.
-
What services are covered.
-
The patient’s financial responsibility.
-
Preauthorization or referral requirements.
Why Is Eligibility Verification Important?
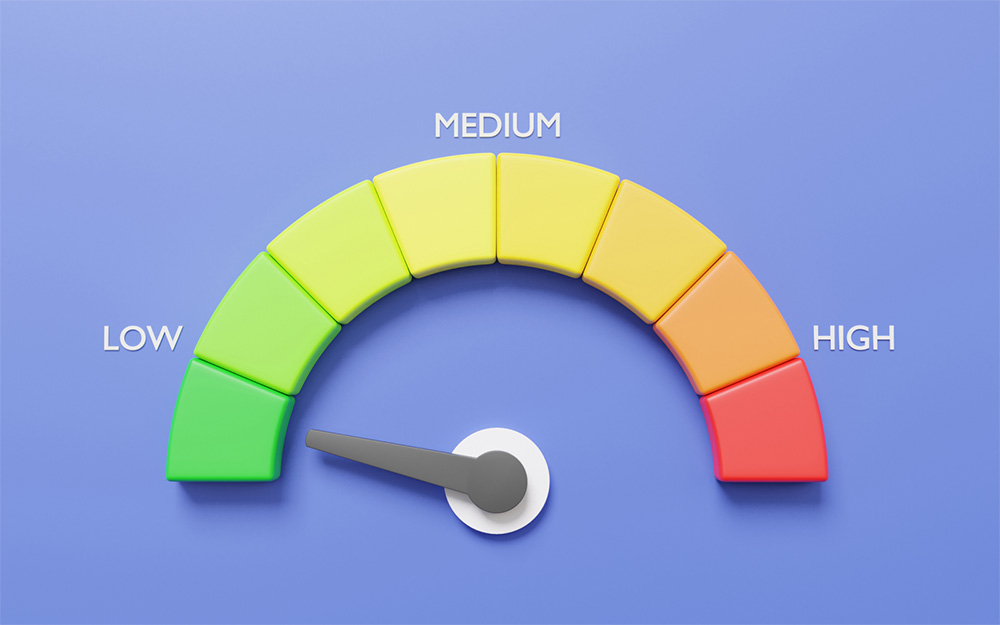
Failing to verify a patient’s insurance eligibility can lead to:
-
Claim denials due to inactive or expired coverage.
-
Delayed payments from insurance providers.
-
Surprise bills for patients.
-
Increased administrative costs for reprocessing claims.
According to industry data, around 25–30% of medical claims are denied due to eligibility issues that could have been caught early in the billing cycle.
Step-by-Step: The Eligibility Verification Process
Let’s take a look at how the eligibility verification process works from start to finish:
1. Collect Patient Information
The process begins at the time of scheduling or check-in. Front desk staff collects:
-
Patient name and date of birth
-
Insurance provider and ID number
-
Group number
-
Contact information
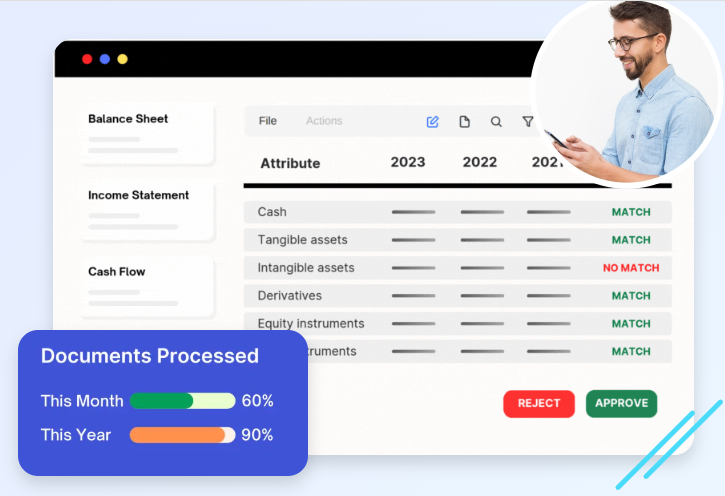
2. Verify Insurance Details
The staff or medical billing team verifies insurance information through:
-
Insurance company portals
-
Real-time eligibility (RTE) software
-
Clearinghouses
-
Manual phone calls (if necessary)
This step includes checking:
-
Coverage start and end dates
-
Plan type and benefits
-
Copayment and deductible amounts
-
Referral or authorization requirements
3. Review and Document
All gathered data is reviewed for accuracy and documented in the patient’s Electronic Health Record (EHR) or Practice Management System (PMS). Any discrepancies or coverage issues are flagged and addressed before the visit.
4. Communicate with Patients
If any issues are identified—such as lack of coverage or high deductibles—patients are informed ahead of time. This helps in setting expectations regarding out-of-pocket costs and payment responsibilities.
5. Follow Up for Changes
Insurance details can change frequently. It’s a best practice to re-verify coverage before every visit, especially for recurring appointments or long-term treatments.
Common Tools Used in Eligibility Verification
Several tools and technologies streamline the verification process, such as:
-
Electronic Health Records (EHR) systems
-
Practice Management Software
-
Insurance portals (payer websites)
-
Clearinghouses
-
Real-time eligibility (RTE) APIs
By automating parts of the process, these tools reduce errors and free up staff for higher-level tasks.
Best Practices for Efficient Eligibility Verification
To ensure a smooth verification process, medical practices should adopt the following best practices:
-
Verify insurance at least 48–72 hours before the appointment
-
Use automated tools whenever possible
-
Train front office staff on insurance types and terminology
-
Keep a checklist of frequently verified plans
-
Maintain accurate and updated patient records
Final Thoughts
The eligibility verification process in medical billing may seem routine, but it is the foundation of a healthy revenue cycle. By verifying insurance coverage early, medical practices can significantly reduce claim rejections, boost patient satisfaction, and optimize revenue. In a healthcare system where efficiency and accuracy are everything, eligibility verification stands out as a small but powerful step with a big impact.


 English
English